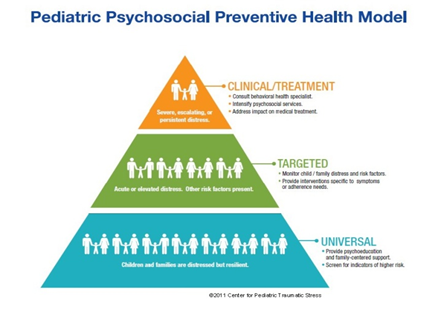
Levels of risk and trauma-informed care
In providing trauma-informed care, not every child and family will need the same level of support.
- The majority will benefit from psychoeducation, comfort, and basic assistance.
- A smaller number with acute distress will need interventions that help address severe emotional distress and support medical adherence.
- Only a few families with severe distress will need mental health treatment.
Healthcare providers can use the Pediatric Psychosocial Preventive Health Model (PPPHM) to guide assessment of psychosocial risks and inform clinical decision making.
Similar to a public health prevention model, trauma-informed care can be grouped into three distinct levels of risk or need, each with differing implications for intervention.:
- UNIVERSAL PSYCHOSOCIAL CARE: Research shows that the majority of ill or injured children and families are distressed but resilient. They need information, comfort, and support in mobilizing their own resources. The D-E-F framework is an excellent guide to helping children and families help themselves after medical trauma.
- TARGETED PSYCHOSOCIAL CARE: A smaller number of children and families with acute distress may need to be monitored and may require interventions that focus on reducing symptoms of traumatic stress or promoting adjustment or adherence to medical treatment.
- CLINICAL PSYCHOSOCIAL CARE / TREATMENT: Only a small minority of children and families will experience distress severe enough to impede active medical treatment. These families may require intensified psychosocial services and/or mental health treatment.
A "Universal precautions" perspective suggests keeping in mind that prior traumatic experiences may shape the responses of ANY child (or parent) facing a new medical event.
Ideally, both psychoeducation and screening are incorporated Universally in the care of all ill or injured children and their families. When providing care through a trauma-informed lens, screening for medical traumatic stress allows health care providers to briefly assess risk status or distress / symptoms and provide children and families with the appropriate level of care. Many screening measures are designed to be administered by frontline providers, or for self-administration by children or parents. After an initial screening, elevated levels of psychosocial risk may indicate the need for additional assessment.
A more in-depth assessment is generally conducted by a provider with mental health training (psychologist, psychiatrist, clinical social worker, or other another clinical mental health provider). The goal of the assessment process is to provide the healthcare team with a clearer picture of the needs and strengths of the child and family and determine the need for Targeted or Clinical* level interventions. In some cases, it will be appropriate to refer to a mental health provider.
Levels of risk and next steps in trauma-informed care
The PPPHM helps guide interpretation of screening and/or assessment results to determine an appropriate plan of care.
- Provide psycho-education and trauma-informed/family-centered support
- Monitor child/family distress and risk factors
- Provide interventions specific to symptoms and adherence needs
- Intesify psychosocial services
- Address impact on medical treatment
- Provide trauma-specific interventions